
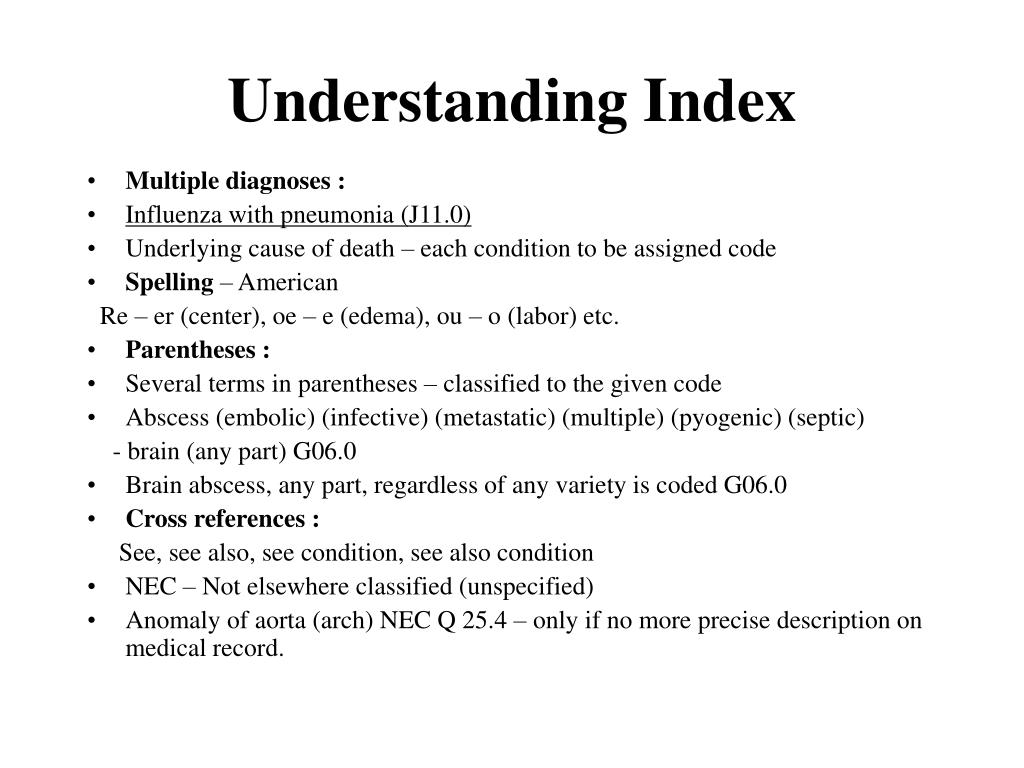
There are a variety of downfalls that can beset providers and MA plans when confronted with a RADV audit. Noncompliance with documentation requirements can lead to legal and financial risks to the health plan, the company, the providers, and coders! Cancers, MI, CVA, TIA, etc.) or Manifestations, ie Diabetes with Neuropathy TIP: Some conditions require specific MEAT to confirm new or active status (e.g. TIP : A minimum of one of the above MEAT components is required
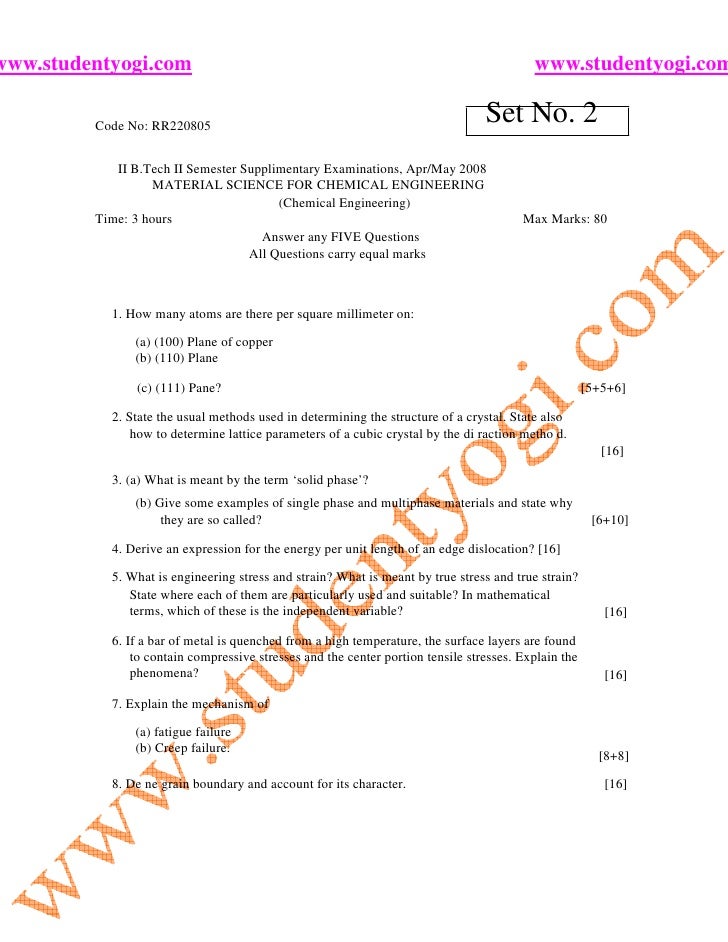
TREAT- Medications, Therapies, Other Modalities. ASSESS/ADDRESS- Ordering Tests, Discussion, Review Records, Counseling. EVALUATE- Test Results, Medication Effectiveness, Response To Treatment. MONITOR-Signs, Symptoms, Disease Progression, Disease Regression. cancer, MI, CVA, TIA, PE, etc.) What does MEAT stand for? What is the answer and what can you as a Provider do within your practice to ensure that the codes submitted to these MA Plans under investigation are correct? Here is a list of best practices to ensure that your practice’s HCC/ICD 10 diagnosis coding is accurate: THE WHO/WHAT/WHEN OF MEAT: Was the condition Monitored, Evaluated, Assessed or Treated?Īll conditions captured must be supported by MEAT or the required specific MEAT for certain conditions (e.g. It all boils down to the data collection process, which of course always points back to the physician’s office and the documentation of the patient encounter. The downstream effect of all this is now that United, Humana, Freedom, Aetna and others are under investigation by the DOJ, is there could be potential practice audits, depending on what comes out as the cases move forward. Which is why you get these letters requesting you review charts or requests to allow their staff into your EMR to comb the patient records to look for “missing/dropped” diagnoses. It is not a large profit margin for the plans, so they chase every dollar possible. The reason for this, is so that if the patient definitely has these conditions, you as the provider, need to correctly report these to the MA Plan, at minimum once per year, so that the Plan can receive enough money from CMS to cover that member’s costs. What they are really asking is if you can quantify these “more severe Chronic Conditions”, like Congestive Heart Failure, or Diabetes with Neuropathy, or Chronic Kidney Disease Stage 4 or higher, as they have somehow been a part of the patients reported past disease history or there is a medication prescribed that could indicate one of the Chronic Conditions being sought for validation by the MA Plan. You participate in several MA Plans and you receive a letter with a list of your patients from the MA Plan asking you to verify some “conditions/diagnoses” that their coders/auditors/software, etc., noticed might be current Chronic Conditions. Let’s say you are a Primary Care Doctor, with a few providers in your practice. 
PRIMARY CARE AND DON’T CARE – WHY YOU SHOULD

Please click on the following link for further information:
M.E.A.T. GUIDELINES MEDICAL CODING CODE
The DOJ also alleges that United provided incentives to participating providers, in order to have them code members for higher severity chronic conditions than what was originally diagnosed.
The problem is that when the coders found these conditions, many have been alleged to not have the required face to face visit. The scheme, tasked their coding team to purposely code patients for “high risk”, “long term” chronic diseases, via data mining of their participating provider member panels for any evidence/mention of any of these within the medical record.
United implemented it as an attempt to significantly improve its overall operating income by close to $100 million. An excerpt from Sheppard Health Law, states that the lawsuit alleges that back in 2010, United Healthcare, organized and implemented a company wide upcoding scheme, which United called “Project 7”.





 0 kommentar(er)
0 kommentar(er)
